20-second summary: Not all wisdom teeth need to be removed. Choosing between active monitoring or extraction depends on your symptoms, the tooth’s position, and its relationship to the nerve. If surgery is needed, we plan it so that recovery is fast and aesthetic.
The essentials: what they are and when they cause problems
Wisdom teeth (third molars) usually erupt between ages 17 and 25. Sometimes they come in properly and cause no trouble; other times they remain partially covered by gum or impacted in the bone. When should we worry?
- Warning signs: recurring pain, swollen gum behind the last tooth, bad taste, difficulty cleaning, cavities on the back of the second molar, or cysts.
- Risk positions: when they “push” against the second molar (mesioangular) or come in halfway (partially erupted), they tend to cause problems.
👉 If you prefer the short version, here’s our direct guide on wisdom teeth: when to stop monitoring and move on to extraction (step by step and with practical tips).
Active monitoring vs. extraction: how to decide
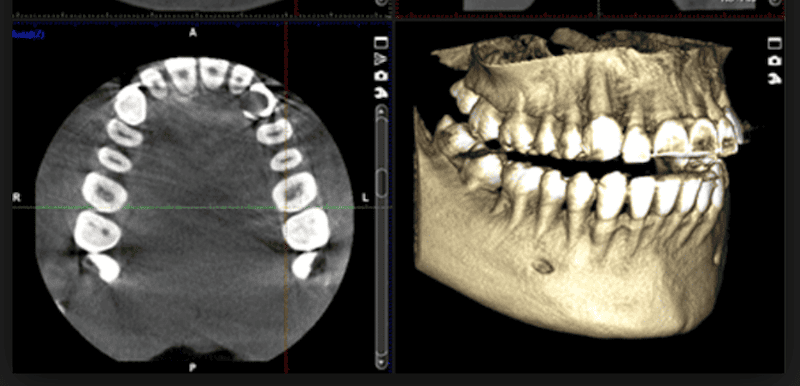
We make the decision with a clinical exam + X-rays. Normally, we start with a panoramic; if there are important doubts (for example, a nearby nerve), we use 3D imaging (CBCT) to decide with precision.
Decision path (in simple terms):
- Is there pain, repeated infections, or cavities in the second molar caused by the third? → Usually indicates extraction.
- Is it impacted, without communication with the mouth and without pathology? → Active monitoring (check-ups + periodic X-rays) may be enough.
- Does the root appear very close to the nerve on the panoramic X-ray? → We assess with CBCT to fine-tune the plan and choose the safest technique.
- Is the risk of touching the nerve high? → There’s the alternative of a coronectomy (removing the crown and leaving the roots so we don’t get close to the nerve; indicated only in very specific cases).
This decision-making approach is aligned with the Clinical Practice Guideline of the Spanish Society of Oral Surgery (SECIB), which prioritizes observation when there is no pathology and recommends extraction when there are signs of disease or damage to the second molar. (See Sources below).
Safe planning (with CBCT when it adds value)
The panoramic X-ray is the first step. CBCT (3D) isn’t ordered “just in case,” but when it changes decisions: for example, to see distances to the inferior alveolar nerve or the shape of the roots and adapt the technique. That’s how we make surgery more predictable and conservative.
- Meet us and see how we integrate advanced diagnostics into the plan: Our specialists.
- What do we use CBCT for in different treatments? We explain it in this educational article on 3D diagnostics and bone health: Oral health and bone diseases.
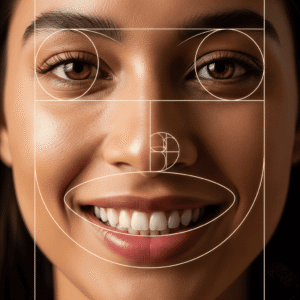
Aesthetic and functional recovery with no surprises
Post-op “aesthetic” checklist:
- Intermittent ice for the first 24–48 hours and sleep with your head elevated.
- Cold/soft diet at first (yogurt, non-acidic smoothies, lukewarm soups).
- Gentle hygiene (avoid brushing the area on the first day); alcohol-free rinses when we indicate.
- No smoking: it stains, causes inflammation, and slows down healing.
- Check-up at 7–10 days to assess tissues and remove stitches if they’re not dissolvable.
Can you see the scar? The incision is made inside the mouth, so it won’t show when you smile. We take care of the gum contour to preserve its shape.
Extra tip: if you’re concerned about the social side (photos, work), schedule your surgery for a time without events and give 72 hours for the swelling to go down visibly.
One or all four at once? Conscious sedation and timing
- Remove one or all? It depends on your case and your schedule. Doing several in the same visit can shorten the overall process, but the first 2–3 days will require more rest.
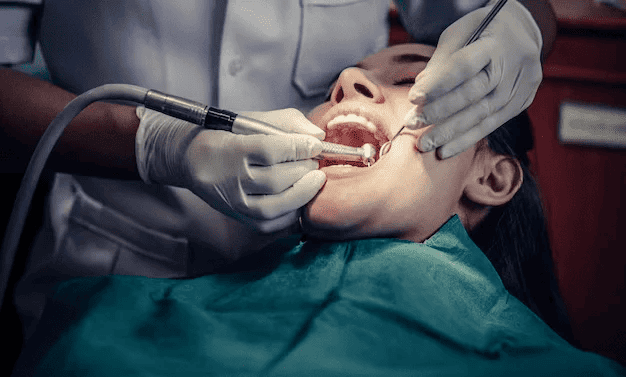
- Conscious sedation? If you feel anxious, sedation helps you relax and cooperate while keeping normal breathing; it feels like “time flies.” Learn how we use it here: Dental anxiety: how conscious sedation transforms your visit.
In our specific wisdom teeth guide, we explain the real timelines and how we organize the appointment to make it as comfortable as possible: Read guide.
Ideal age & cost-benefit
At younger ages, the bone is usually more flexible and the roots less developed, which makes surgery and recovery easier. But it’s not just about age: what really matters is the tooth’s position and its relationship to the nerve. That’s why we personalize: observation when it’s stable and problem-free, extraction when it’s already causing issues or very likely to do so.
Frequently Asked Questions
How do I know if I need an extraction or just monitoring?
If there’s pain, repeated infections, or cavities in the second molar caused by the third, we usually recommend extraction. If it’s impacted and problem-free, active monitoring (check-ups + X-rays) may be enough.
When do you request a CBCT (3D)?
When the panoramic X-ray suggests proximity to the nerve or the anatomy is unclear and we need to determine technique and risks with precision.
What is a coronectomy?
In selected cases with high neurological risk, we remove only the crown and leave the roots to avoid getting too close to the nerve. This doesn’t apply to all patients.
How long does the surgery take and what does it feel like?
Depending on complexity, about 15 to 45 minutes. With local anesthesia (and sedation if you choose it), it’s usually very manageable. Swelling peaks between 48–72 hours and then improves.
Need help deciding?

- Schedule an evaluation with our specialists.
- Check out our services and get answers in the AM Dental Studio blog.
- If you already have a recent panoramic X-ray, bring it; if a CBCT is needed, we’ll explain why and what for.
Sources and recommended readings
- SECIB Clinical Practice Guideline (2023): Diagnosis and indications for third molar extraction. A reference document that supports the approach of monitoring vs extraction and when to consider CBCT or coronectomy. Download PDF
- Our blog: