When the oncologist confirms that you need chemotherapy, the last thing that usually crosses our mind is scheduling a dental appointment. However, that “minor” visit can prevent painful sores, fever, delays in medication, and even the loss of several teeth. This article—designed for patients and families—explains, in clear language and with some depth, why the mouth plays a key role before, during, and after cancer treatment.
1. Chemotherapy doesn’t distinguish good from bad cells (and the mouth feels it)
Chemotherapy works because it attacks tissues that reproduce quickly. The problem is that the cells of the oral mucous, hair roots, and bone marrow also divide very rapidly. Under normal conditions, the microdamage in the mucous heals almost unnoticed, thanks to saliva—a “natural gel” full of enzymes, minerals, and antibodies.
When the drug takes effect, the protective film of saliva decreases, cell regeneration slows down, and the microbial balance is disrupted. The result usually shows up in three ways:
- Xerostomia (dry mouth): the salivary gland produces less fluid; you lose the feeling of moisture, the tongue scrapes against the palate, and speech becomes sticky.
- Mucositis: the layer of cells covering the cheeks, gums, lips, and tongue becomes inflamed, red, and often develops whitish sores.
- Opportunistic infections: fungi like Candida albicans or cariogenic bacteria take advantage of the weakened defenses to multiply with much less immune opposition.
All this doesn’t just hurt: an infected ulcer can force the oncologist to lower the chemotherapy dose or delay an entire cycle. That’s why it’s so important to start treatment with the mouth in the best possible condition.
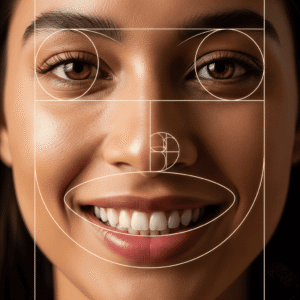
2. The “saliva–enamel” circuit: how dryness causes rampant cavities
Perhaps the side effect I emphasize most to my patients is xerostomia because it triggers the rest of the problems. “Without saliva— I always explain—your mouth loses both its self-cleaning and self-repair systems.”
- Self-cleaning: every time you swallow, a small stream of saliva carries away food debris, neutralizes acids, and sweeps bacteria. If that flow dries up, plaque sticks more firmly and the pH takes much longer to return to neutral levels.
- Self-repair: the minerals in saliva (calcium, phosphate, and fluoride) “re-seal” microfractures in the enamel caused by acid. Without this exchange, the outer layer of the tooth becomes porous, dull, and extremely vulnerable.
In healthy adults, a crown cavity can take 2–3 years to break through the enamel. In patients with severe xerostomia, I’ve seen “rampant” cavities worsen teeth in just three months. Reaching the pulp during chemotherapy complicates everything: anesthesia that doesn’t coagulate the same, bacteremias, antibiotics that interfere with cancer medication… Better to prevent it from the start.
3. Pre-chemotherapy dental checkup: what is done and when to schedule it

The “dentist’s view” before chemo is not just looking at the mouth with a little mirror. It consists of four well-measured steps:
a) Medical history and selective X-ray
⚬ Your medication, allergies, and blood count are updated.
⚬ A periapical or panoramic X-ray is taken to rule out hidden cavities, apical infections, or fractured roots.
b) Professional cleaning and polishing
⚬ We remove tartar and hard plaque that irritate the gums.
⚬ We polish rough surfaces so that plaque takes longer to reaccumulate.
c) Sealing of “fixable” problems
⚬ Fillings, small root canals, fractured crowns… anything that can heal and recover within 10–14 days is treated before the first cycle.
d) Strategic extractions
⚬ Teeth with no possible prognosis—severe mobility, chronic infection, vertical fracture—are extracted at least 14 (preferably 21) days before starting chemo. This time allows the bone to form a solid clot and the gum to close without complications.
When to book your appointment: as soon as you know the date of your first cycle. If you’re short on time, the most urgent step is to control infections and remove the “time bomb teeth”; small fillings can wait until the first window of higher immunity between cycles.
4. Safe treatments and those best postponed
| Timing | Recommended treatments | Treatments to avoid unless absolutely urgent |
|---|---|---|
| Pre-chemo (3–2 weeks before) | Cleaning, fillings, crowns, necessary extractions, fluoride varnish | Dental implants, bone graft surgeries |
| Between cycles (when neutrophils > 1,000–1,500) | Prosthesis adjustment, mucositis management, topical fluoride | Invasive surgery, deep subgingival scaling |
| Nadir days (very low count) | Only emergencies with antibiotic coverage and hospital monitoring | Any procedure that bleeds for more than 30 seconds |
Practical note: your dentist will request the full blood count from the oncologist to choose the ideal day. The more communication there is between them, the fewer surprises you’ll encounter.
5. Xerostomia: 4-front battle plan
1. Constant hydration
Carry a small thermos and take sips every 10 minutes; don’t wait until you’re “thirsty.” Lukewarm water soothes the mucous and helps with swallowing.
2. Saliva stimulation
Sugar-free gum, xylitol lozenges, or gels with malic acid increase pressure on the glands and trick your brain into producing some saliva. Two hours a day chewing or sucking can make a huge difference.
3. Nighttime lubrication
There are pharmacy gels or moisturizing sprays made with carboxymethylcellulose and glycerin. Apply them before bed; you’ll wake up with a less sticky mouth and reduce trauma from the tongue against the palate.
4. Enamel strengthening
5% fluoride varnishes (22,600 ppm) applied in the clinic every three months, plus 1,500 ppm toothpaste at home, remineralize enamel and slow down aggressive cavities.
“Saliva is your invisible armor; without it, teeth are left uncovered. If we can’t generate saliva, we must mimic its functions.” –Explanation I give to every patient before handing out the xerostomia kit.
6. Daily care step by step (detailed version)**
- Toothbrush: ultra-soft bristles, small head. Replace every 4 weeks.
- Toothpaste: without sodium lauryl sulfate (SLS)—the foaming agent that can irritate sores. Look for 1,450–1,500 ppm fluoride.
- Dental floss: waxed and flat. Glide gently; if the gum bleeds, it’s inflammation, not a “cut.”
- Mouthwash: daytime, neutral rinse with xylitol; nighttime, 0.05% fluoride. Avoid alcohol-based rinses (they dry out more).
- Tongue scraper: gently drag from back to front. Reduces bacterial load and bad breath.
- Diet: five mini-meals instead of two feasts. Choose soft textures without much sugar or acidity (pasta, white fish, avocado, green smoothies).
7. Mucositis and candidiasis: how to detect and relieve them
Mucositis
- Early sign: shiny gum, dark red color.
- Prevention: rinses with cold saline water (1 tsp salt / 250 ml) four times a day, crushed ice 10 min before and 30 min after infusion (oral cryotherapy).
- Treatment: if ulcers appear, the dentist may prescribe hyaluronic acid gel or mallow/aristosidone rinse twice a day.
Candidiasis
- Symptom: white tongue, metallic taste, “sandpaper” sensation when swallowing.
- Prevention: maintain neutral pH with sips of water and sugar-free dairy.
- Treatment: nystatin suspension or miconazole gel for 7–14 days.
With these steps, more than 70% of patients control lesions without interrupting chemo.
8. Practical cases – what I’ve seen in practice
Case A: Carolina, 34 years old, Hodgkin’s lymphoma
- Called five days before the first cycle, with a deep cavity in a lower molar.
- An express root canal and provisional crown were done.
- At 15 days, leukocytes at 800; mild mucositis, controlled with chamomile rinse and bicarbonate solution.
- Completed six cycles without extra hospitalizations or delays.
Case B: José, 56 years old, gastric carcinoma
- Did not see the dentist before chemo.
- By the second cycle he developed pericoronitis in an impacted wisdom tooth.
- Pain + fever; oncologist delayed one cycle and lowered the dose.
- He ultimately lost two molars and needed a bone graft after remission.
Moral: what seems like “just one tooth” can disrupt the entire oncology schedule.
9. FAQ for patients and families

Can I whiten my teeth before treatment?
Not recommended: peroxide gels irritate the gums and increase sensitivity.
What if I’ve already started chemo and notice tooth pain?
Call the dentist immediately: an X-ray will be taken, and if needed, treatment will be scheduled during the highest immune window with preventive antibiotics.
Does saliva return to normal after chemo?
In most cases yes, although it may take two to six months. In the meantime, follow the hydration and fluoride protocol.
Will I need antibiotics for every cleaning?
It depends on your neutrophil count. If it’s below 1,000 and the cleaning will cause significant bleeding, yes; in other cases, a disinfectant mouthwash is enough.
10. Conclusions: a small appointment for a huge benefit
A simple dental checkup, done with at least two weeks’ notice, can save you from infections, reduce the severity of mucositis, and prevent your oncologist from having to postpone your treatment. Remember:
- Dry mouth + plaque = cavities and painful sores.
- Necessary extractions should be done before starting chemotherapy.
- Fluid communication between dentist and oncologist = less risk and less anxiety for you.
Schedule your checkup as soon as the date of your first cycle is confirmed. Bring a list of your current medications and share your questions without fear: nothing is “too silly” when it comes to your health. With your mouth in perfect condition, you’ll have one less concern and can focus on what really matters: overcoming cancer with the best possible quality of life.